Immune thrombocytopenia types
Last updated June 26, 2025, by Lindsey Shapiro, PhD

There are a few different ways to classify the autoimmune bleeding disorder immune thrombocytopenia (ITP), and identifying which type a person has can help doctors decide how the condition needs to be monitored and treated.
ITP arises when the immune system erroneously attacks and destroys the body’s own healthy platelets, which are cell fragments needed for blood clotting. Patients typically experience low platelet symptoms like easy bruising or bleeding.
The main types of immune thrombocytopenia — primary ITP and secondary ITP — differ in whether the disease occurs secondarily to another underlying condition. ITP can also be classified based on how long it has lasted and its severity.
Understanding how ITP is classified is important for making informed treatment decisions that ensure the best possible outcomes for people living with ITP.
Main types of ITP
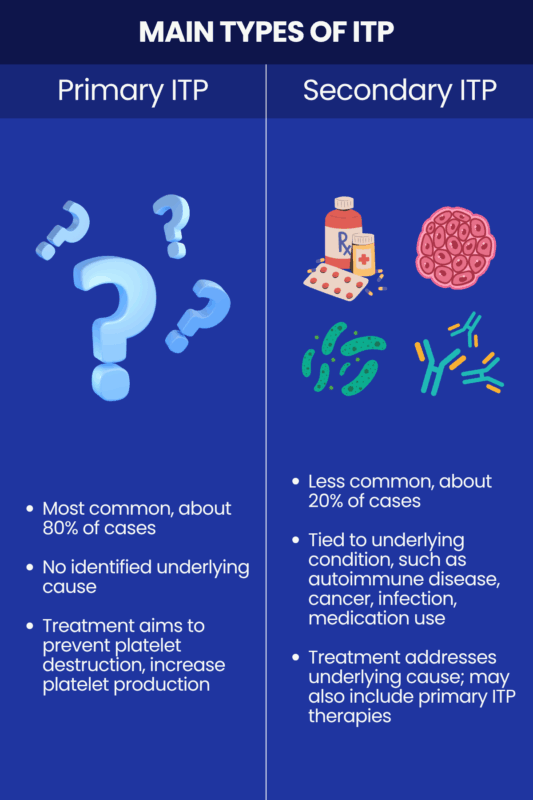
All cases of ITP are characterized by the immune system’s mistaken attack on platelets. Sometimes there is no known cause for this, and sometimes an underlying condition can be identified. This difference forms the basis between the two main ITP types:
- In about 80% of cases, the cause of ITP is not known, and it is called primary or idiopathic ITP.
- In as many as 20% of cases, ITP occurs secondarily to an underlying condition, which is referred to as secondary ITP.
All people with ITP have low platelet counts that impair blood clotting, leading to easy bruising and bleeding. As such, ITP symptoms are generally similar regardless of the disease type. However, it is still very important to identify whether the condition is primary or secondary when reaching an ITP diagnosis, as they may be treated differently.
Primary ITP
Most people with ITP have the primary form of the disease, in which no underlying ITP causes can be identified. This type of ITP is most common in young children and older adults. In adults, it occurs more often in women.
In some milder cases, primary ITP may not be treated at first, but will instead be monitored to see if it resolves on its own. When medication is needed, the main goal of first-line ITP treatment is to suppress the immune system’s mistaken platelet destruction. This can be done via:
- corticosteroid medications
- intravenous (into-the-vein) immunoglobulin
- anti-D immunoglobulin.
If this doesn’t work to ease signs of a low platelet count, there are various other second-line therapies to stimulate platelet production or prevent platelet destruction. Sometimes, a person may undergo a splenectomy, or surgery to remove the spleen, which is where platelets are destroyed in ITP.
People with primary ITP generally have a good prognosis with proper management, and a life expectancy that is not drastically reduced relative to the general population.
Secondary ITP
Secondary ITP occurs when there are external ITP triggers that alter immune function in ways believed to promote antiplatelet attacks. Possible triggers for secondary ITP include:
- viral or bacterial infections
- other autoimmune diseases
- certain cancers, particularly blood cancers like leukemia or lymphoma
- some medications
- vaccinations, though this is rare.
Secondary ITP is likely more common in adults than children due to the higher prevalence of underlying conditions like autoimmune diseases and cancer in this older age group.
While the symptoms of secondary ITP are largely the same as those of the primary type, people with this form of the disease may also experience other symptoms related to the underlying condition that caused ITP.
A primary focus of secondary ITP treatment is to manage the underlying disease that triggered it, for example, eradicating an infection or treating a blood cancer. ITP-specific treatments such as those used for primary ITP may also be used at the same time, especially if a person’s platelet counts get very low.
Some studies show that the prognosis for secondary ITP is generally somewhat worse than for primary ITP.
ITP classification
Beyond the two main ITP types, doctors may further classify ITP based on how prolonged and severe its symptoms are. This can guide clinicians in making treatment and management decisions.
Disease duration
For some people, ITP resolves on its own in the short term, but for others, it can be more persistent. The disease can thus be broadly grouped based on how long symptoms have lasted since a person’s diagnosis. Most recently, this classification includes:
- newly diagnosed ITP, or the first three months after diagnosis
- persistent ITP, when symptoms continue for three months to a year
- chronic ITP, where symptoms last for more than a year.
Some sources have historically referred to ITP simply as acute if it lasted less than six months, or chronic if it persisted for longer than that.
In general, younger children are found to be more likely to experience acute ITP that resolves without treatment within a few months and doesn’t come back. Chronic ITP may have symptoms that come and go. It more often occurs in adults, and is 2-3 times more common in females than in males.
Among people with ITP, this classification can affect treatment decisions. For newly diagnosed patients, spontaneous remission is possible, so patients may be monitored without treatment if they don’t have severe symptoms. With persistent or chronic ITP, spontaneous remission becomes less likely and treatment is often needed at some point to keep platelet levels up.
Disease severity and treatment responsiveness
ITP may also be classified based on how severe it is and how well it has responded to treatment.
The condition is considered severe when:
- a person has clinically relevant bleeding symptoms at disease onset that are substantial enough to require treatment
- new bleeding symptoms arise that require additional treatment with a new therapy or an increased dose.
ITP may also be referred to as refractory, or treatment-resistant, if the following criteria are met:
- a person has severe ITP or a risk of bleeding that requires treatment, and
- a splenectomy did not work to control the disease.
Splenectomies are not as commonly performed to treat ITP as they used to be. As such, in some cases, people who failed to respond to multiple therapies, regardless of whether they’ve had their spleen removed, may be considered refractory.
Some sources also use the term mild ITP to refer to forms of the disease in which there are no significant bleeding symptoms and where treatment is often not required.
How ITP varies in children and adults
These ITP types and classifications apply to both children and adults, and the symptoms are generally the same across all ages. Still, the disease tends to manifest differently in adult vs. pediatric ITP.
- Adults are more likely than children to have secondary ITP related to an underlying condition.
- ITP in children is usually short-term and resolves spontaneously without treatment.
- ITP in adults is more likely to be persistent or chronic and require treatment.
Bleeding Disorders News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- US scientists create tool to predict chronic ITP in children
- US supporters urged to ‘Go RED’ this Bleeding Disorders Awareness Month
- Red blood cell therapy may promote immune tolerance in iTTP: Study
- Epstein-Barr virus infection triggers severe ITP in woman, 18: Report
- Veyvondi effective, reduces costs, as VWF replacement therapy: Study
Related articles
-

-

THROMBOTIC THROMBOCYTOPENIC PURPURA
NewsRed blood cell therapy may promote immune tolerance in iTTP: Study
-
-
-
THROMBOTIC THROMBOCYTOPENIC PURPURA
NewsBrazil study shows early diagnosis is key to better outcomes in TTP