Bleeding risk high soon after kidney transplant in VWD, hemophilia A
Study offers insight into feasibility of renal procedure for these patients
Written by |
People with von Willebrand disease (VWD) or hemophilia A are more likely to experience serious bleeding in the first month after a kidney transplant, a new study from researchers at Mayo Clinic in Arizona suggests.
After this early period, the risk of bleeding decreases, but later risks — including clotting-related complications and organ rejection — remain. Still, the rates of these events mirrored those seen in people without bleeding disorders who undergo the same procedure.
“The study provides valuable preliminary insight into the feasibility of renal transplantation in patients with bleeding disorders,” researchers wrote, while emphasizing the need for close, long-term monitoring.
The study, “Characteristics and posttransplant outcomes of patients with congenital and acquired von Willebrand disease and hemophilia A and with renal transplants,” was published in Research and Practice in Thrombosis and Haemostasis.
Survival has improved for hemophilia patients
Hemophilia A, the most common form of hemophilia, and VWD are bleeding disorders that impair the body’s ability to form blood clots, leading to abnormal or prolonged bleeding. Both can cause frequent nosebleeds, easy bruising, and bleeding after injury or surgery.
In the past, people with hemophilia had shortened life expectancy due to serious bleeding episodes and infections acquired through blood infusions. Survival has since improved dramatically, and many patients now live long enough to develop age-related conditions such as diabetes, high blood pressure, cancer, and kidney disease.
As these conditions progress, some eventually require major surgeries — including organ transplant — which carry added risks for people with bleeding disorders.
“Nevertheless, large-scale studies evaluating renal disease progression and transplant outcomes in this population are lacking,” the researchers wrote. “As therapeutic advances continue to improve outcomes for patients with bleeding disorders, it is increasingly important to understand the unique challenges and outcomes associated with renal transplantation in this population.”
Bleeding was dominant complication early after surgery
To help address this gap, researchers reviewed outcomes from 11 adults who underwent a kidney transplant between 2003 and 2024, representing 12 transplant episodes. Most participants were male (63.6%) and white (81.8%), with a mean age at the time of transplant of 59 years old.
Three patients (27.3%) had a diagnosis of hemophilia A, while the remaining eight patients (72.7%) were diagnosed with VWD — six with the acquired form and two with inherited VWD type 1.
All participants had anemia, a condition in which the body lacks enough healthy red blood cells or hemoglobin to carry oxygen, and 81.8% had high blood pressure. Other health issues included thrombocytopenia, characterized by low platelet counts, in 36.4% of patients, and thrombocytosis, marked by elevated platelet levels, in 27%. Platelets are cell fragments that play a crucial role in blood clotting.
Liver disease was reported in three individuals (27.3%), one of whom later required a liver transplant. Three (27.3%) had diabetes, and three (27.3%) had a history of cancer.
These findings underscore that although risk diminishes after the immediate postoperative period, long-term vigilance remains essential.
The median time spent on the transplant waitlist was 355 days. One participant (9%) underwent a simultaneous liver-kidney transplant, while the other 10 received kidney-only transplants. Slightly more than half (54.5%) received kidneys from living donors, while 45.5% received kidneys from donors who had died.
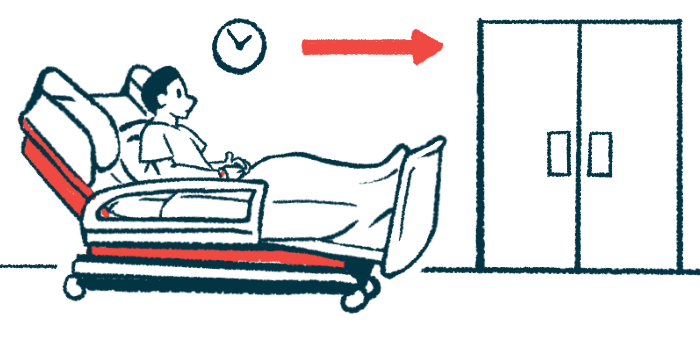
Bleeding was the dominant complication early after surgery. Within the first 30 days, about one month, five patients (45%) experienced a bleeding event, with four of these (80%) classified as major. Acute bleeding events were most frequently perinephric hematomas, or blood around the transplanted kidney. Severe, extensive bleeding during surgery occurred in the one patient who received both a liver and a kidney.
After this initial period, no bleeding events occurred between 30 and 365 days, or about one year. However, bleeding occurred again in four patients (36%) after the first year, mainly due to problems in the digestive tract rather than issues involving the transplanted kidney.
“These findings underscore that although risk diminishes after the immediate postoperative period, long-term vigilance remains essential,” the team wrote.
Clotting issues arose more than a year after surgery
Clotting-related issues followed a different pattern. While none occurred during the first year after transplant, four patients (36%) developed clotting-related complications beyond the one-year mark, including two heart attacks, two deep vein thromboses (a blood clot that forms in a deep vein, typically in the legs, causing pain and other symptoms), and one ischemic stroke.
“These outcomes mirror observations in [non-bleeding] disorder transplant populations, where cardiovascular disease remains a major late complication,” the researchers wrote.
Two patients (18%) required a second surgery, either for transplant-related issues or other surgical complications.
Hospital readmission was common during the early stages of recovery. Four patients (36%) returned to the hospital within the first month, and three (27%) were readmitted between one and three months, for reasons including kidney injury or infections. Between three months and one year, readmission dropped to 9.1%.
Three patients (27.3%) experienced transplant rejection, most commonly acute rejection (18.2%). This rate was consistent with what is typically seen in kidney transplant recipients without bleeding disorders, especially within the first six months after surgery, the researchers noted. Five patients (45%) died during follow-up.
“Renal transplantation can be safely performed in patients with bleeding [predisposition], with acceptable perioperative [disease risk],” the researchers wrote. “Although bleeding is the dominant risk early after surgery, late [clotting-related] events emerge as clinically significant. Close multidisciplinary follow-up is therefore critical to optimize both patient and [transplant] outcomes.”