Immune thrombocytopenia overview
Last updated Sept. 4, 2025, by Lindsey Shapiro, PhD

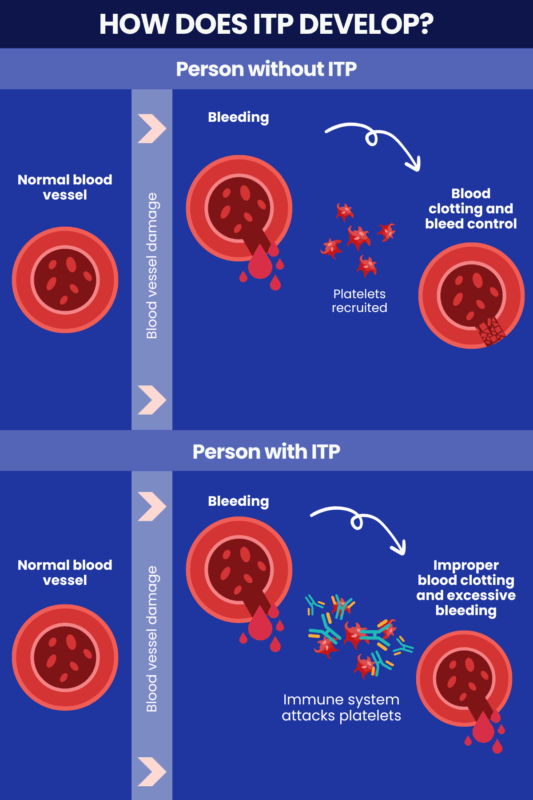
Immune thrombocytopenia (ITP) is a rare autoimmune disorder marked by a loss of platelets, or the circulating cell fragments needed to help blood clot after an injury, leading to various forms of internal or external bleeding.
While many of its symptoms can be mild, appropriate ITP diagnosis and treatment is key to avoid rare, but possibly serious or life-threatening bleeding events.
There’s no cure for ITP, but the disease can go into a state of remission where platelet counts are stable and the risk of bleeding is greatly reduced. With a proper monitoring and treatment plan in place, many people with ITP have a relatively normal life expectancy.
What is ITP?
In ITP, the immune system attacks and destroys the platelets that play a vital role in clotting blood and stopping bleeding after an injury. A lack of platelets — medically known as thrombocytopenia — leaves a person at risk for easy bruising and bleeding.
ITP affects children and adults. It can resolve on its own within a few months to a year, especially in children. Other times, it persists long term and requires treatment to keep platelet counts up and the risk of bleeding down.
People with ITP can have periods of remission, where the disease is under control even without treatment, interspersed with relapses, where platelet levels drop and treatment is needed.
The disease was previously known as idiopathic thrombocytopenic purpura, but a group of experts recommended the nomenclature be updated in 2009 to more accurately reflect understanding of the disease.
ITP is a rare disease, with an annual incidence in the U.S. of around 3.3 per 100,000 people. It is estimated that more than 200,000 people are living with ITP worldwide.
Causes of ITP
Platelet destruction in ITP happens when immune B-cells and plasma cells produce antibodies that bind to platelets, marking them for destruction by immune macrophages in the spleen. These antibodies can also target platelet precursors in the bone marrow to inhibit platelet production. It is not known exactly what causes the immune system to launch these attacks.
In about 80% of cases, no underlying condition or other factor is associated with ITP. This is known as primary, or idiopathic, ITP. The remaining patients have secondary ITP, where an underlying condition is associated with disease development. Secondary ITP causes include:
- viral or bacterial infections
- other autoimmune diseases
- certain cancers, particularly blood cancers
- some medications
- vaccinations
- pregnancy.
Other factors may also influence the risk of ITP, including age, sex, or exposure to possible triggers. ITP is overall more common in children, and is more likely to occur in girls than boys starting in adolescence.
Types of ITP
ITP is largely classified into two main types — primary ITP and secondary ITP — based on whether or not the disease is associated with an underlying trigger. These ITP types have similar symptoms, but may be managed differently.
Primary ITP
In primary ITP, no underlying disease cause is identified. It:
- is the most common form in young children and older adults
- occurs more often in women than in men during adulthood
- is monitored closely or treated with standard ITP therapies.
Secondary ITP
In secondary ITP, an external trigger alters immune function in ways believed to promote ITP disease processes, including certain other diseases, infections, and medications. This form of ITP:
- is more common in adults than in children
- can have additional symptoms related to the underlying condition
- is treated by addressing the underlying trigger, and with ITP therapies as necessary.
Other classifications
ITP is sometimes further classified as newly diagnosed, persistent, or chronic, based on how long symptoms have lasted. It may sometimes be referred to simply as acute ITP or chronic ITP.
The disease is also classified as severe when bleeding symptoms require treatment at diagnosis, or new symptoms arise that require an escalation in treatment. ITP is considered to be refractory (treatment-resistant) when it is severe and doesn’t respond to certain treatment approaches.
Symptoms of ITP
The symptoms of ITP arise mostly from an increased risk of internal or external bleeding due to low platelet counts. If platelet counts are high enough to keep the risk of bleeding low, a person may not have any ITP symptoms.
As platelet counts decline and bleeding risk increases, possible symptoms include:
- easy or excessive bruising or bleeding, even after a minor injury
- red, purple, or brown spots or patches on the skin or in the mouth, known as petechiae and purpura
- hematoma, or clotted blood under the skin that can look like a lump
- bleeding from the gums or blood blisters in the mouth
- frequent or difficult-to-stop nosebleeds
- unusually heavy or prolonged menstrual bleeding
- fatigue.
Very low platelet counts can also raise the risk of more serious bleeding, including internal bleeding in vital organs. Signs of such complications could include:
- blood in the urine, stool, or vomit
- severe or persistent abdominal pain
- neurological symptoms, such as severe or persistent headaches, confusion, dizziness, blurred vision, weakness, or unexplained drowsiness.
ITP diagnosis
ITP is considered a diagnosis of exclusion, meaning it mainly relies on ruling out other possible causes of a low platelet count or bleeding symptom. It’s also important to distinguish between primary and secondary ITP, as this can affect how the disease is treated.
The process may involve:
- collecting a thorough medical history
- a physical exam
- blood tests to measure platelet counts and other blood components
- monitoring responses to ITP treatment
- a bone marrow biopsy, in certain situations.
Reaching a prompt and accurate diagnosis is key to ensure that ITP is properly monitored and managed so that platelet counts don’t get so low as to cause significant bleeding.
ITP treatment
Guidelines for ITP treatment depend on a variety of factors, including a person’s age, symptoms, lifestyle, ITP type, and treatment history.
If there are no notable bleeding symptoms and platelet counts pose no risk of clinically significant bleeding, managing ITP through careful monitoring may be preferred over active treatment.
In other cases, medications may be needed to keep platelet levels up and the disease at bay.
First-line treatments to prevent platelets from being destroyed by the immune system include:
- corticosteroids for ITP, such as dexamethasone and prednisone
- intravenous immunoglobulin, with several brands available
- anti-D immunoglobulin, including Rhophylac and WinRho SDF.
When response to initial therapies is insufficient, second-line treatments may be required. Some of these treatments work to stimulate the production of new platelets in the bone marrow, while others work in different ways to prevent platelet destruction. These include:
- thrombopoietin receptor agonists, including Alvaiz (eltrombopag tablets), Doptelet (avatrombopag), Nplate (romiplostim), or Promacta (eltrombopag)
- rituximab
- splenectomy, or surgery to remove the spleen
- Tavalisse (fostamatinib disodium hexahydrate)
- Wayrilz (rilzabrutinib).
Life expectancy and prognosis
While there is no cure for the rare bleeding disorder, people living with ITP can lead full and active lives with appropriate monitoring and treatment.
In general, ITP life expectancy does not differ significantly from the general population, although the mortality rate in adult patients is slightly higher than what’s seen in their peers. It is rare to die from ITP, and disease-related deaths are mainly associated with bleeding complications.
ITP prognosis can be influenced by other factors, such as:
- prompt and accurate diagnosis and treatment
- disease severity, duration, and treatment responsiveness
- age, with children generally having a shorter, self-resolving disease course and an overall better prognosis than adults
- disease type, with some studies finding that life expectancy for primary ITP is better than for secondary ITP.
Bleeding Disorders News strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Experimental VWD treatment HMB-002 shows promise in animal models
- African ancestry linked to 50% higher iTTP relapse risk after rituximab
- Seeing my rare disease highlighted on TV brings validation and hope
- Managing anxiety levels may improve quality of life for adults with ITP: Study
- Many types of von Willebrand disease may be underdiagnosed: Study
