Immune thrombocytopenia diagnosis
Last updated June 24, 2025, by Lindsey Shapiro, PhD

There’s no single test that can definitively diagnose immune thrombocytopenia (ITP). Rather, reaching an ITP diagnosis relies on multiple evaluations to rule out other possible causes of low platelet counts and bleeding symptoms, which are the hallmarks of the disease.
In ITP, the immune system mistakenly destroys the body’s own healthy platelets. These cell fragments are needed for blood clotting, so their deficiency — medically known as thrombocytopenia — leaves a person susceptible to easy or excessive bruising and bleeding.
Reaching an accurate and early ITP diagnosis — and identifying any known disease triggers — is important for ensuring that the disease is appropriately monitored and treated. Sometimes, a positive response to ITP treatment helps confirm the diagnosis, while a lack of response could warrant further evaluation.
Importance of an early diagnosis
For people with ITP, a delayed or inappropriate diagnosis could mean a person goes longer without the right treatment, increasing the risk that their platelet levels will get low enough to cause significant bleeding. It’s also important to know if there’s an underlying trigger for ITP, as these conditions on their own can lead to other complications if left unmanaged.
Ultimately, an early ITP diagnosis ensures that patients receive the right care promptly, maximizing the chances of successful treatment before any serious complications might occur. In turn, this can help maintain a relatively normal ITP life expectancy and a good life quality.
Initial evaluation and diagnostic criteria
ITP may be suspected when a person experiences ITP symptoms, such as easy bruising or bleeding. Some people with ITP do not have any symptoms, but a low platelet count is incidentally found during blood work done for another reason.
The disease exists in two forms:
- primary ITP, where there’s no known ITP causes
- secondary ITP, where ITP occurs in the context of another external cause, such as another autoimmune disease, infections, blood or bone marrow disorders, or medication use.
It’s important to distinguish between primary and secondary ITP during the diagnostic process, as this will affect how the disease is managed. It’s also important to rule out other conditions that could be causing thrombocytopenia and that need to be treated differently.
An ITP diagnosis is thus generally considered a “diagnosis of exclusion,” which means its diagnostic criteria center around ruling out other possible low platelet count causes.
This process usually involves:
- a thorough medical history examination to evaluate bleeding symptoms, possible secondary ITP triggers or causes, or other medical conditions that could cause bleeding
- a physical exam to look for signs of bleeding consistent with ITP
- blood tests to measure platelet counts and other blood components
- monitoring responses to ITP treatments.
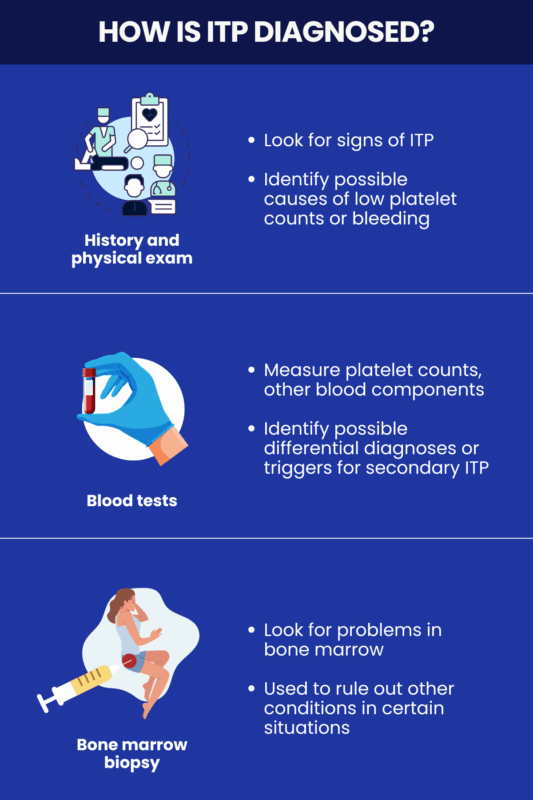
Blood tests
Blood tests are the cornerstone for reaching an ITP diagnosis, as they’re used to measure platelet counts and rule out other possible causes of thrombocytopenia. There’s no single definitive ITP blood test, but a few tests together can help hone in on a diagnosis. These include:
- a complete blood count (CBC) to provide a detailed picture about the numbers of various blood cell types, including red blood cells, white blood cells, and platelets
- a peripheral blood smear, where a small drop of blood is spread thinly and examined under a microscope to assess the size and shape of a person’s blood cells, if a CBC looks abnormal
- a reticulocyte count that measures the number of immature red blood cells in the blood to help evaluate the function of the bone marrow, where platelets and other blood cells are made, and rule out other conditions
- infection screening to look for infections linked to secondary ITP, such as HIV, hepatitis C, or Helicobacter pylori.
Together, these tests may point toward an ITP diagnosis. ITP is generally marked by isolated thrombocytopenia, where a platelet count test shows that platelet levels are unusually low, but red and white blood cells are normal in number, size, and shape.
Abnormalities in those cells could suggest a different diagnosis. For example, certain white blood cell changes could suggest the blood cancer leukemia.
Sometimes, platelet antibody tests are used to identify autoimmune thrombocytopenia. Tests for antibodies linked to other autoimmune diseases may also be performed. However, anti-platelet antibodies are not seen in every ITP patient and some guidelines don’t recommend routinely performing such tests.
Bone marrow examination
A bone marrow biopsy is an invasive procedure that involves inserting a needle and collecting a small sample of bone marrow for analysis. In ITP, the bone marrow itself is usually healthy.
This procedure is no longer routinely performed for diagnosing ITP in adults or children if they have a typical disease presentation. It may be used in certain situations to rule out other conditions, particularly in older adults. Such circumstances may include cases where:
- the diagnosis is uncertain
- an ITP blood smear shows signs of blood-related abnormalities other than thrombocytopenia
- a person doesn’t respond to standard ITP treatments.
Diagnostic differences between adults and children
In general, the fundamental process for diagnosing ITP in children and adults is similar, relying heavily on medical history and blood tests to exclude other possible diagnoses. Still, there are some subtle differences, such as:
- a bone marrow biopsy may be more commonly done in older adults, ven thoough it isn’t widely used anymore in adults or children
- testing for infectious agents like HIV, hepatitis C virus, and H.pylori is not routinely done in children, but is recommended for adults.
Other differential diagnoses could be more or less likely in adult and pediatric populations, so a healthcare provider will also consider those in deciding which tests are appropriate.
Bleeding Disorders News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Experimental VWD treatment HMB-002 shows promise in animal models
- African ancestry linked to 50% higher iTTP relapse risk after rituximab
- Seeing my rare disease highlighted on TV brings validation and hope
- Managing anxiety levels may improve quality of life for adults with ITP: Study
- Many types of von Willebrand disease may be underdiagnosed: Study
