ITP complicates man’s benign tumor surgery: Case study
Doctors remove spine tumor after stabilizing platelet counts
Written by |
Doctors found that immune thrombocytopenia (ITP) complicated the surgical removal of a slow-growing, benign tumor along the spine of a 28-year-old man that impaired his motor function.
They were able to remove most of the tumor — a type called a myxopapillary ependymoma, or MPE — after his platelet counts normalized with second-line IPT treatments, and his walking ability improved.
“This patient’s initial presentation with ITP in the context of MPE is unique,” the researchers wrote. “The patient’s ITP may have resulted in intra-tumor bleeding.”
They described the case in the study, “Myxopapillary ependymoma complicated by immune thrombocytopenia and intraoperative diabetes Insipidus: A case report,” published in Interdisciplinary Neurosurgery.
In ITP, the immune system mistakenly attacks platelets, small, disk-shaped cell fragments found in the bloodstream that help blood clot after injury. Such attacks reduce platelet counts, medically known as thrombocytopenia, and increase the risk of bruising and bleeding.
Small spots prompt emergency visit
The previously healthy 28-year-old man arrived at the clinicians’ emergency department with petechiae, small, flat spots of bleeding under the skin. Blood tests revealed severe thrombocytopenia, with platelet counts of 3,000 per microliter (normal range: 150,000-450,000 per microliter).
After receiving first-line corticosteroid and intravenous immunoglobulin for presumed ITP, the man’s platelet count improved to 146,000 per microliter, and he was discharged.
Less than a week later, however, he returned to the hospital with nosebleeds and a parastehsia (a feeling of numbness, tingling, or burning in the legs). Doctors found he had sensory loss in his legs, an exaggerated muscle reflex, and impaired muscle coordination.
MRI revealed a tumor inside the membrane surrounding the spinal cord in the chest area, alongside fluid buildup. There was also a minor lesion in his right tentorium (a fold of membrane that separates two brain regions, the cerebrum and cerebellum).
He was readmitted to the hospital due to the severe thrombocytopenia that wasn’t adequately controlled by the initial treatment, as well as progressive leg weakness and impaired walking.
Doctors needed to normalize the man’s platelet counts before he was able to receive surgery to remove the tumor. He was treated with Nplate (romiplostim), a second-line ITP therapy designed to boost platelet production, which normalized his platelet counts after several doses.
With stable platelet counts, he was able to undergo a biopsy of the tumor and a laminectomy, surgery to ease pressure on the spinal cord and nerves of the lower spine.
“This patient’s severe thrombocytopenia posed a significant obstacle to the standard therapy of tumor resection,” the team wrote. “Until his platelet count normalized, surgical intervention was postponed.”
An examination of the tumor tissue revealed a grade 2 MPE, a rare, slow-growing, and typically benign (non-cancerous) tumor that originates in the lower spine. Common symptoms include low back pain, leg weakness, and problems with bowel/bladder function.
The man underwent a second surgery through the back to open the middle part of the spinal canal to relieve pressure on the spinal cord and remove most of a tumor inside the spinal cord’s protective covering. After removing the tumor, the surgeon repaired the membrane using a biologic patch.
During the procedure, however, clinicians discovered multiple tumors attached to the spinal cord and nerve roots, preventing a complete removal of tumor tissue.
The procedure was also complicated by diabetes insipidus, a rare condition characterized by excessive urination and frequent thirst, which was resolved with appropriate treatment. The man also experienced pain caused by the incision and developed Ogilvie’s Syndrome, a severe widening of the colon without a physical blockage. Both were successfully treated.
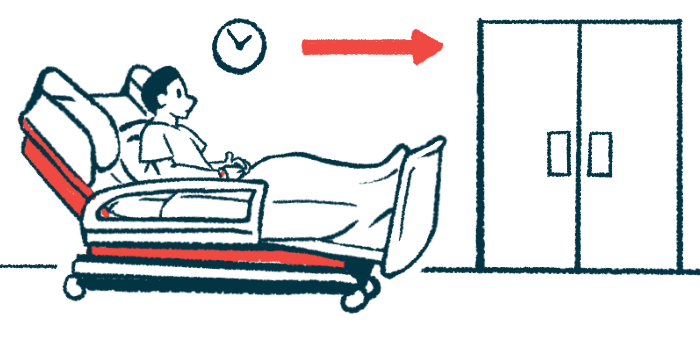
His leg strength, gait, and balance continued to improve, and after 18 days, he was discharged to an acute rehabilitation facility and eventually home. He still had residual tumor tissue, but additional surgery was ruled out, and he underwent radiation therapy.
Eighteen months after the surgery, the man was able to walk without assistance, and sensation in his legs had improved substantially, with MRI scans showing stable disease. After Nplate stopped working, the man switched to Alvaiz (eltrombopag tablets), another second-line ITP therapy that boosts platelet production.
“Patients with ITP have a higher overall risk for cancer, especially gastrointestinal, skin, lymphoid, and hematological [blood] cancers compared to the general population,” the researchers wrote. “Although the relationships between ITP and [diabetes insipidus] with MPE have not been extensively documented, these relationships should be further investigated as they may have implications for prognosis and treatment options.”